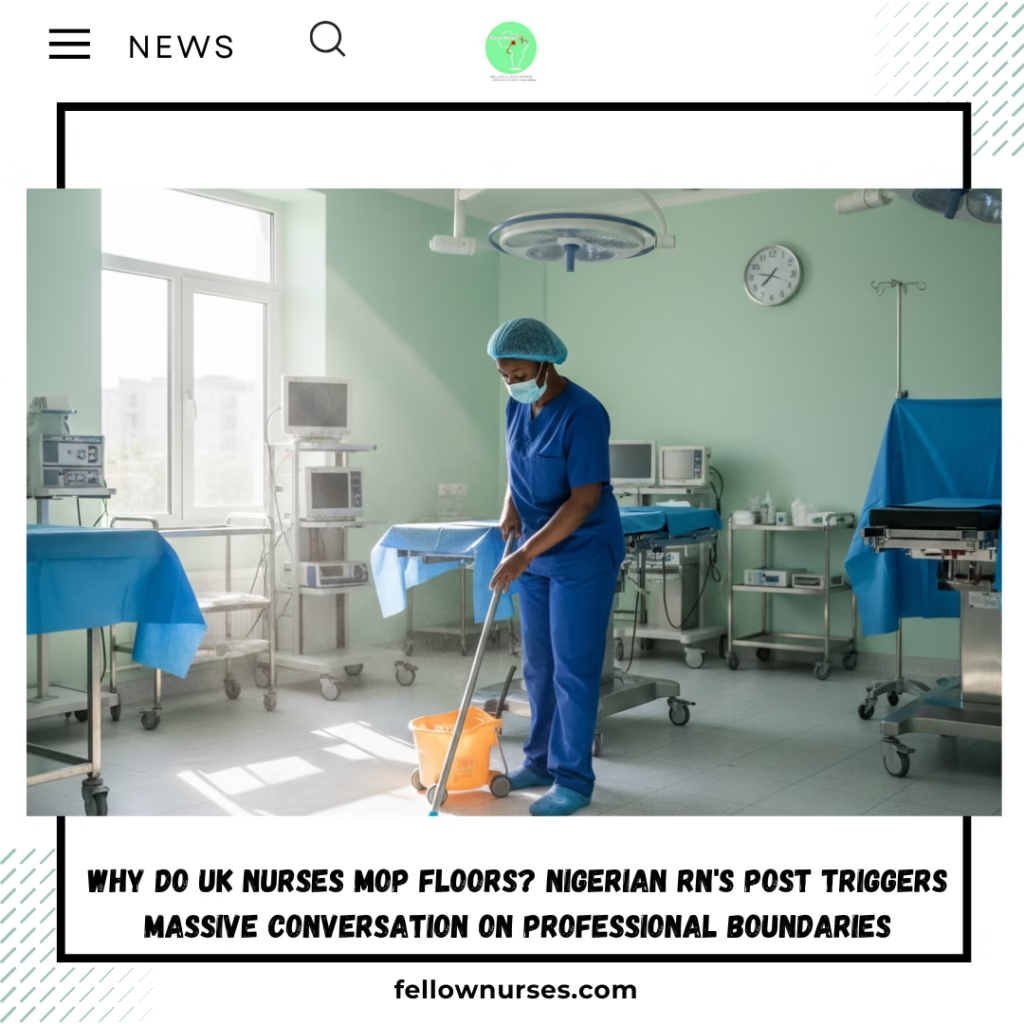
Why Do UK Nurses Mop Floors? Nigerian RN’s Post Triggers Massive Conversation on Professional Boundaries
A viral social media post by a Nigerian-trained registered nurse working in the UK’s National Health Service (NHS) has sparked widespread debate among healthcare professionals about the scope of nursing duties in operating theatres.
The nurse, who shares her experiences under the handle @proudnursemj on X (formerly Twitter), described her surprise upon discovering that theatre nurses in the UK are routinely involved in cleaning tasks, including mopping floors after surgical procedures.
In her detailed account, posted on 28 January 2026, she explained that during her time as a registered nurse in Nigeria, strict role separation meant nurses focused exclusively on clinical responsibilities. Health technicians handled equipment preparation and dismantling, while dedicated cleaners performed post-operative environmental cleaning, including floor mopping.
Upon joining an NHS operating theatre in 2019, she recounted asking about cleaners after a case, only to learn that the nursing team itself carries out “damp dusting” and mopping to prepare the room for the next patient. She described grabbing the mop from her team leader on her first day, stunned by the expectation in what she viewed as a highly advanced healthcare system.
👉 Join our Whatsapp channel Here
The post, which has garnered hundreds of thousands of views, hundreds of replies, reposts and quotes, frames the issue not as personal reluctance but as a question of professional boundaries: “If a system trains nurses as clinicians… why use them as cleaners?”
The Reality of Theatre Turnover in the NHS
Perioperative nursing in UK operating theatres involves a range of responsibilities during patient preparation, surgery and recovery. Theatre nurses (often Band 5 registered nurses or operating department practitioners) assist surgeons, manage instruments, monitor patients and ensure aseptic technique.
Between cases, rapid theatre turnover is essential to maintain surgical schedules and reduce waiting times. This includes “clean down” procedures: wiping surfaces, removing waste, damp dusting equipment and mopping floors, particularly when blood or bodily fluids are present. NHS guidelines, including the National Standards of Healthcare Cleanliness 2025, emphasise that high-risk areas like operating theatres require thorough disinfection to prevent healthcare-associated infections.
While domestic services staff (typically Band 2 domestic assistants or housekeepers) handle routine cleaning in many hospital areas, operating theatres often restrict access to non-clinical personnel during or immediately after procedures due to infection control risks and the need for specialised handling of biohazards. Clinical staff, including nurses, frequently perform or assist with these tasks to ensure quick, safe turnover. Official NHS documents and perioperative guidelines note that nursing teams contribute to cleaning responsibilities in theatres, especially for immediate post-case decontamination.
This practice contrasts with more stratified systems in some countries, including Nigeria, where dedicated cleaners or technicians manage such duties.
Broader Implications and Expert Perspectives
The post has resonated with many internationally recruited nurses, particularly from Nigeria, the Philippines and India, who form a significant portion of the UK’s nursing workforce amid ongoing shortages. Many describe similar “culture shocks” upon arrival, including expanded non-clinical duties driven by staffing pressures.
Experts in perioperative care highlight the tension between efficiency and role specialisation. Rapid turnover supports patient access to surgery but can contribute to workload strain and perceptions of role erosion for highly trained clinicians.
The Royal College of Nursing and Association for Perioperative Practice (AfPP) advocate for clear role definitions, adequate staffing and recognition of nursing as a clinical profession. Chronic shortages in the NHS—exacerbated by post-pandemic demands—often lead to “all-hands” approaches in high-pressure environments.
Advocates for migrant nurses argue that better induction support, transparent expectations during recruitment and policies to protect clinical time could ease transitions and reduce burnout.
The conversation underscores ongoing challenges in the NHS: balancing infection prevention, operational efficiency and professional respect in an under-resourced system.
Diverse Reactions from the Nursing Community
Responses to the post reflect a range of perspectives, highlighting both support for the concerns raised and defences of UK practices:
- Several commenters, including UK-based and migrant nurses, agreed that strict role separation in Nigeria protects clinical focus, with one noting: “Most Nigerians do cleaning work in UK even worse than mopping ground. But… a nurse that stayed for hours in the theatre should finish and start mopping again… It’s not normal.”
- Others criticised perceived double standards, with a medical doctor observing: “All of a sudden a professional nurse mopping the theatre is now a ‘cultural thing’… I have never seen a nurse mopping the theatre floor in any of our teaching hospitals in Nigeria.”
- Some emphasised systemic differences without judgment: “Nurses have different role in different part of the world. In Nigeria, cleaners do the cleaning. In the UK nurses do the cleaning so I don’t think she’s fussing. It’s just systemic differences.”
- A few pointed to broader issues, including one user stating: “A registered nurse don’t have any business mopping floors after operation. It doesn’t make any sense for them to.”
👉 Join our Whatsapp channel Here
The varied viewpoints illustrate the complexity of adapting to different healthcare models, with many calling for greater dialogue on role clarity and support for internationally trained staff.
Fellow Nurses Africa will continue to monitor reactions and related discussions within the nursing community.
👉 Join our Whatsapp channel Here
Fellow Nurses Africa is the independent voice of African nursing, we educate, inform and support nurses across Africa
This article draws on publicly available NHS guidelines, perioperative standards and verified social media content for factual accuracy.