Fellow Nurses Africa | Lagos, Nigeria | 18 November, 2025
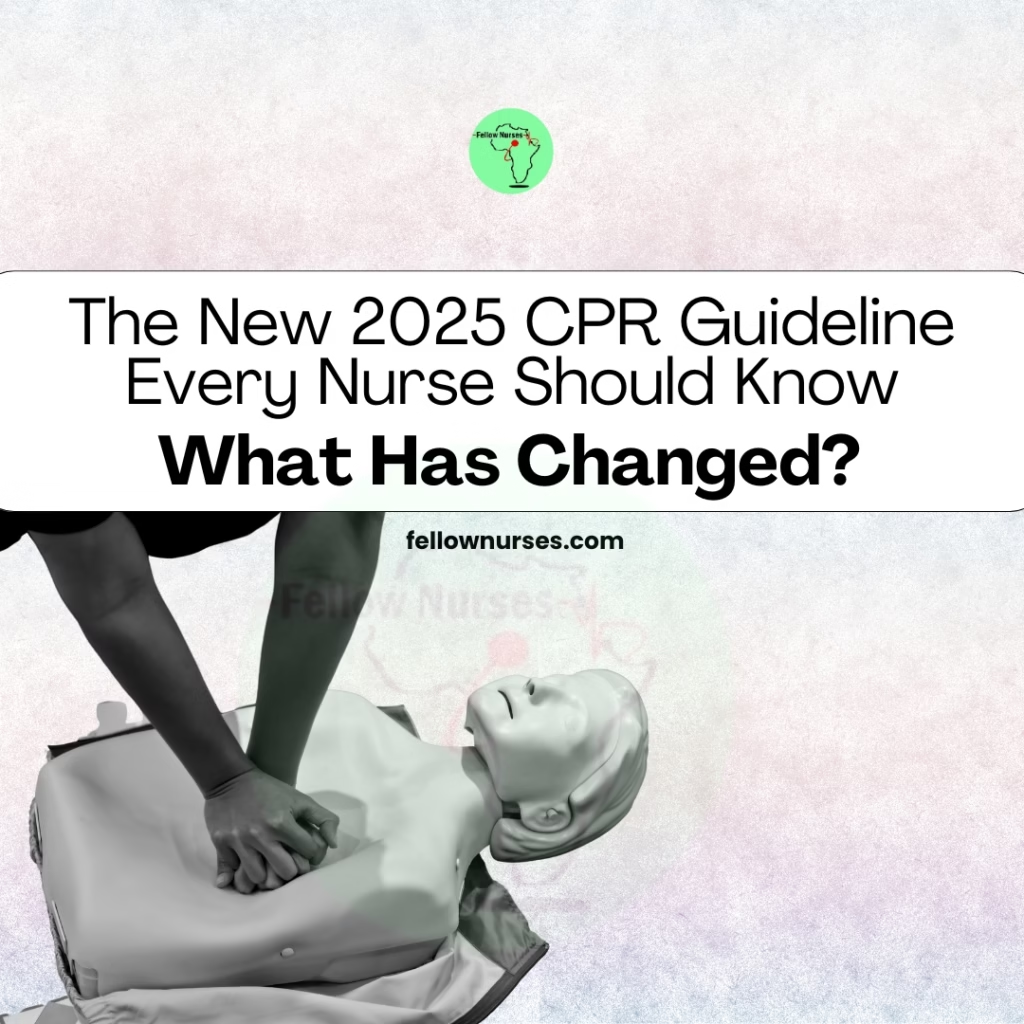
In October 2025, global resuscitation councils released the most comprehensive update to CPR and emergency cardiovascular care (ECC) since 2020.
These revisions reflect new science, real-world data, and persistent challenges in emergency response from choking and opioid overdose to poor CPR retention among the public and healthcare workers alike.
These updates directly influence bedside care, emergency response workflows, community teaching, and clinical decision-making.
This article breaks down the key changes, why they matter, and what nurses must start doing differently today.
1. A Unified “Chain of Survival” for All Cardiac Arrests
The 2025 guidelines introduce a major conceptual change: a single, universal Chain of Survival.
Previously, chains differed for adult vs paediatric, or in-hospital vs out-of-hospital cardiac arrest. This often created confusion during training or code blue events. The new unified chain highlights:
- Early recognition
- Early CPR
- Early defibrillation
- High-quality advanced life support
- Integrated post-cardiac arrest care
For nurses working in mixed units (ED, ICU, Med-Surg), this simplifies the mental flow and reduces hesitation during crises.
2. New Choking (Foreign-Body Airway Obstruction) Steps
One of the most notable updates is the new alternating sequence for conscious choking victims.
Adults and Children (Conscious)
Alternate:
- 5 back blows → 5 abdominal thrusts
- Continue this cycle until the object is expelled or the victim becomes unresponsive.
Infants (Conscious)
Alternate: 5 back blows → 5 chest thrusts (using the heel of one hand)
Why the change?
Studies show that combining these maneuvers creates better airway pressure dynamics than using just one method. This significantly increases the chances of clearing the obstruction quickly.
Nursing implications
- Update choking training for patients, families, and the public.
- Modify unit posters, emergency trolleys, and simulation practices.
- For maternity and paediatrics units, ensure chest-thrust techniques are correctly taught and demonstrated.
3. Strengthened Guidance on Opioid Overdose Response
Given rising opioid emergencies globally, 2025 guidelines introduce clearer steps for suspected overdose.
Key points
- Naloxone (opioid antagonist) should be administered rapidly where overdose is suspected.
- Do not delay CPR while retrieving naloxone.
- Ventilation support is emphasised because opioid toxicity primarily causes respiratory depression before cardiac arrest.
Nursing implications
-
Ensure naloxone is in medication kits, ED triage rooms, ambulatory clinics, and community outreach bags.
-
Train all staff (including non-clinical) on recognising opioid overdose signs.
-
Emphasise simultaneous CPR + naloxone when the patient becomes unresponsive with no normal breathing.
4. Mechanical CPR Devices, Not for Routine Use
The guidelines clarify a long-debated topic: mechanical CPR devices should NOT be the default for adult cardiac arrest.
When to consider them
- During prolonged resuscitation
- During transport when manual CPR is unsafe or impossible
- High-risk environments (e.g., cath lab, moving ambulance)
Nursing implications
- Review your facility’s mechanical CPR protocols.
- Practice seamless switchovers to avoid interruptions in compressions.
- Reinforce manual CPR as the gold standard.
5. Paediatric & Neonatal Updates
Updated recommendations developed with the American Academy of Pediatrics address key areas:
- Airway positioning
- Oxygen strategy
- Compression–ventilation ratios
- Drug dosing considerations
- Post-resuscitation stabilization
Nursing implications
-
Maternity, NICU, and emergency nurses should review neonatal and paediatric flowcharts.
-
Simulations should incorporate the updated chest thrust rules for infants.
-
Ensure neonatal resuscitation equipment is aligned with updated oxygen and airway guidance.
6. Early, Accessible CPR Education Starting from Age 4
The guidelines emphasise a generational shift: teach CPR early, teach frequently, and teach in modern ways.
- Education changes
- CPR training recommended from age 4–6 years in schools
- Use of gamified learning, simulations, and rapid-cycle deliberate practice
- Emphasis on frequent refreshers to prevent skill decay
- Instructor transition requirements for AHA-certified trainers
Nurses are among the top CPR trainers in communities, schools, churches, and workplaces. The shift encourages nurses to:
- Modernise teaching techniques
- Use shorter, high-yield training sessions
- Focus on confidence-building instead of memorisation
- Support community-wide CPR literacy
7. Dispatcher-Assisted CPR & Public AED Access
The guidelines strongly reinforce the value of:
-Dispatcher-assisted CPR (phone-guided CPR)
- Removing barriers to AED access
- Public mapping and clear signage for defibrillators
Nursing implications
- Advocate for AED visibility and signage in your workplace.
- Educate patients, caregivers, and community members to never hesitate to use an AED.
- Support updating facility protocols on emergency notification and rapid AED retrieval.
8. Post-Resuscitation Care & Mental Health Support
The guidelines highlight two often overlooked areas:
A. Post-cardiac arrest care
- Temperature control
- Oxygenation and ventilation targets
- Coronary interventions
- Neurological monitoring
- Family involvement in decision-making
B. Psychological impact on rescuers
For the first time, guidelines acknowledge the emotional burden on:
- Bystanders
- Nurses
- Healthcare teams
- Family members who participate in CPR
Systems are encouraged to create post-resuscitation debriefs, provide emotional support, and monitor for psychological trauma.
What Nurses Should Start Doing Now
-
Update your clinical practice
-
Update your unit
-
Update your training materials
-
Strengthen teamwork and mental health support
The 2025 CPR guideline updates reflect the evolving realities of emergency care from opioid overdose and choking emergencies to the psychological weight of life-saving interventions.
Refreshing your knowledge, updating your unit’s protocols, and embracing modern, accessible CPR education will ensure that you are fully aligned with global best practices and prepared to save more lives with confidence.